Support strong Canadian climate journalism for 2025
Erin Edghill ended up in the emergency room last summer for a back injury they say was in part caused by binding their chest for years while waiting for top surgery in Ontario’s public health-care system.
The 25-year-old York University student and queer activist decided not to disclose their trans and non-binary identity to doctors at a Scarborough hospital who were already discrediting the amount of pain they were in and trying to convince them to go home and skip scans because it would not find anything useful.
"I was juggling this dynamic of: 'Do I tell them and out myself, what are the risks with that? Or do I just sit here in silence and get as good care as I can?'" they said in a video interview. “The quality of care is so all over the place already, so you throw in, ‘Oh yeah, I'm trans,’ and you don't know what the outcome is going to be."
In education as much as in health care, the trans population in Ontario remains largely hidden in public data, making it harder to assign resources to address specific challenges.
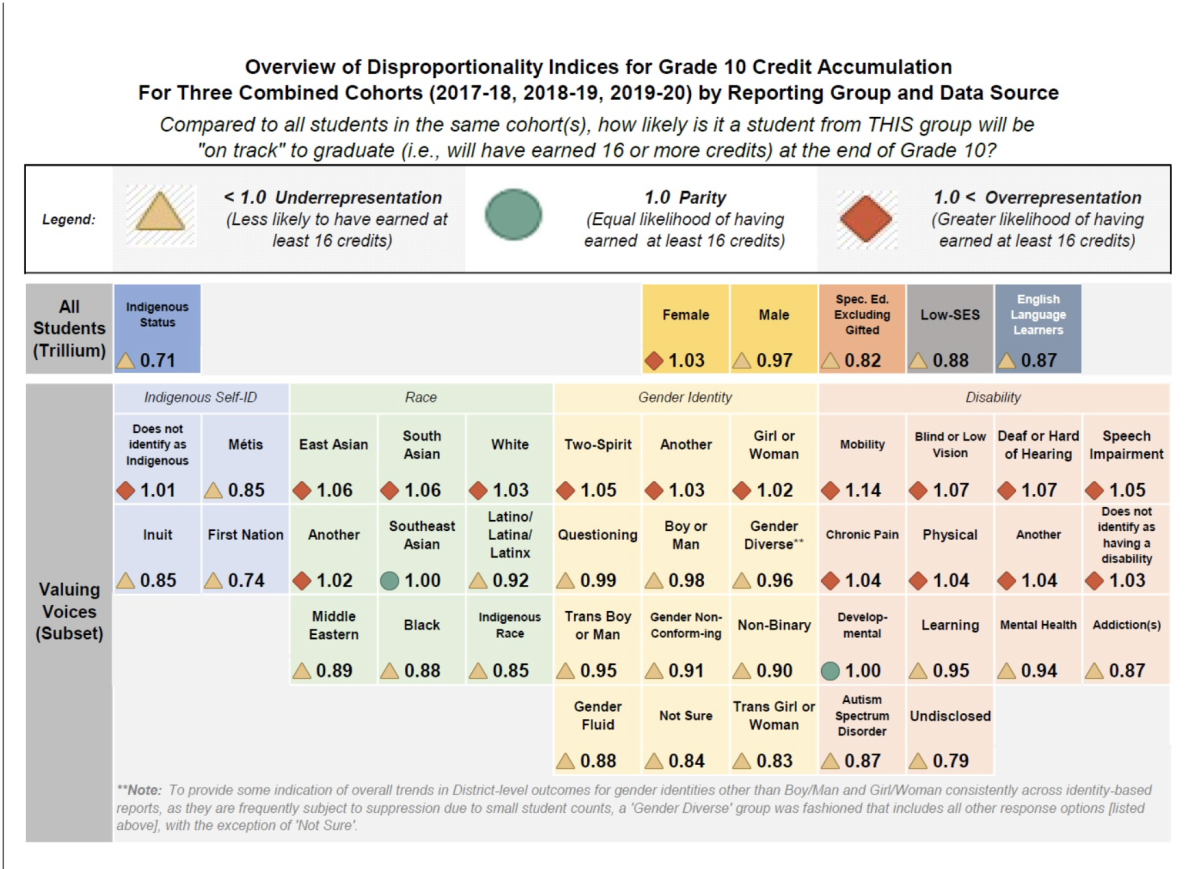
Trans students at the Ottawa-Carleton District School Board are likely to have fallen behind their peers by Grade 10, but Lyra Evans and other trustees can only tell by how much because the board recently conducted its own survey of student demographics.
"If those are the students who are struggling with mental health, if those are the students who are struggling with graduating on time, then we need to put resources towards making sure that all of our students get a fair shake," said Evans, perhaps Canada’s first openly transgender school board trustee.
"But that is something our school board had to undertake on our own, and it’s not something that is mandated in a lot of school boards," she said, pointing to the need for provincial funding earmarked to meet the specific needs of LGBTQ+ students and for boards not to force anyone to out themselves.
"This significant discrepancy between the average and trans students was enough to cause us to hire a trans specific graduation coach," she said.
Trans patients are often invisible in Ontario’s health-care system, but when Dr. Alex Abramovich went looking, he found they were more likely than cis patients to have diabetes, asthma or HIV, or to require mental health services, including dealing with self-harm.
Abramovich trawled through several government databases to build the ongoing health study comparing 2,000 trans patients at specialist clinics in Toronto, Ottawa and Thunder Bay to an age-matched sample of 10,000 from the general population.
Almost 900 of the trans individuals Abramovich surveyed were 24 years old or younger, with a similar number in the 25 to 44 age group.
He says the province’s health-care system needs to work much harder to make them visible in order to serve their health needs.
“Doctors need to ask their patients: ‘How do you identify? And what pronouns do you go by?’” said Abramovich, an independent scientist who works with Toronto’s Centre for Addiction and Mental Health.
Most hospitals and doctors offices routinely collect data on sex designation based on what is listed on a person’s provincial health insurance (OHIP) card rather than gender identity, Abramovich said, making transgender and non-binary people invisible to a system they often struggle to navigate.
“They can’t rely on a person's sex designation on OHIP. It's so important for the medical system to actually collect this type of data so that we can learn more about the trans population and the health needs of trans folks," he added.
Abramovich’s study found people whose gender identity does not align with the sex they were assigned at birth are more likely than others to live in lower-income neighborhoods, experience chronic physical and mental health conditions, and use more health services.
Who gets to know?
Asked on Wednesday’s International Trans Day of Visibility whether the provincial government might consider recording people’s gender identity in health records to better serve their needs, Ontario’s health minister said it’s “something we are looking at.”
“I can't say we're doing it tomorrow, but it is something we are looking at because we know there have been concerns expressed by trans people with respect to that,” said Christine Elliott.
One concern Edghill has is about who gets to see that information.
"I can see it as very useful in data, but if it's something that is carried with you, whether that's in referrals or emergency rooms, I can see it also posing a risk" of receiving a lower level of care or facing direct or indirect transphobia, they said.
"As soon as that information is there, I'm outed, because I was assigned female at birth and I'm on testosterone and I've had top surgery, so there's no opportunity for me to fly under the radar when needed for my own personal safety."
(The type of data Abramovich collated is administrative in nature and did not link gender identity to an individual’s health information except for the data on trans patients drawn from specialist clinics.)
Edghill said if gender identity could be linked to a health card number, but not sit on the card or in a patient’s general medical file, trans patients would have the option of sharing that information or not in clinical settings.
“I think that would provide one way to track the data and use it in really meaningful ways, while also not outing people unintentionally," they said, adding that mandatory training for doctors and medical staff on trans issues would also help reduce tensions and limit misunderstandings.
Studies typically estimate that transgender people make up between 0.5 per cent and 1.3 per cent of the adult population, for a worldwide total of around 25 million.
They also show trans people are medically underserved broadly, and experience ongoing stigma, discrimination, and socioeconomic disadvantages, which lead to poor health outcomes.
The federal government is trying to better collect data on the country’s trans population, and next year’s census will ask about gender identity as well as sex at birth for the first time.
Canada is also conducting a wide-ranging study on LGBTQ2S health, which CAMH’s Abramovich has told a parliamentary committee should include a question on gender identity with a list of response options on all federal surveys.
“People need to see themselves reflected in the programs that they access. People need to see themselves on the forms that they are asked to fill in. It’s not enough to just have male, female or other. No one wants to check off ‘other.’ People want to see their own identity reflected on institutional forms.”
Morgan Sharp / Local Journalism Initiative / Canada’s National Observer






Comments